Article Recap – OR Manager – Day in the Life of SPD
Ambulatory surgery centers (ASCs) are continuing to perform more and more surgical procedures. According to Fortune Business Insights, ASCs can expect to see even greater case volumes as the number of outpatient procedures is estimated to increase by 15% by 2028.
With an increase in procedures, it is essential that ASC staff maintain the proper infection prevention protocols. This is important throughout an entire facility, but especially in the sterile processing department (SPD). For SPD professionals, daily tasks can, and should, be highly detailed. Each step ensures the sterility of the reusable instruments used in an ASC.
Inside look at SPD
Before outlining the day-to-day tasks of the SPD team, note the various areas within the department. The designated areas of an SPD can differ depending on the facility. For example, one facility could have a decontamination/dirty room, a clean room, and sterile storage. Another facility could have a decontamination/dirty room, a clean room, a sterile room, and sterile storage.
Even though the areas may differ per facility, one component always remains the same: there is a defined dirty area and a clean area. These designated areas are in place to prevent cross-contamination and to prevent health care practitioners from choosing contaminated instruments, instead of sterile instruments, for procedures.
Before entering, don PPE
SPD personnel must don the correct personal protective equipment (PPE) before entering the SPD. The Centers for Disease Control and Prevention (CDC) conducted a study in 2016 and found that between 9% and 12% of healthcare professionals did not wear gowns or protective gloves while in the SPD.
PPE that should be worn includes gowns, gloves, goggles, and masks. When donning PPE, it is crucial to wear the correct types and every item at all times until exiting the SPD. This may include regular nitrile, chloroprene, and puncture-proof protective gloves. These gloves help prevent percutaneous injuries while professionals manage the contaminated instruments. After the SPD personnel don the proper PPE, it is time to enter the SPD.
Phase 1: Soaking
Within each room, different equipment is used to clean contaminated instruments. A day in the life starts in the decontamination/dirty room. In this room, there is typically a soak/holding sink, a wash sink, a rinse sink, an automated instrument washer, and an ultrasonic cleaner. The soak/holding sink contains a pre-soak solution that helps prevent bioburden from sticking to the instruments. These solutions predominately use an enzymatic solution to prevent bioburden from drying. Sometimes technicians cannot process instruments right after the procedure. When this happens, the personnel will place the instruments in the soak sink. When it is time to process the instruments, SPD personnel will take the instruments from the soak sink and move them to the next phase.
Phase 2: Cleaning
Phase 2 is cleaning the instruments. There are two methods used for cleaning: manual and automated. Manually cleaning the instruments will be done in the wash sink. The manual method is excellent for instruments that may not withstand the ultrasonic cleaner and instrument washer.
Instruments that can withstand ultrasonic cleaners and instrument washers can be placed in the automated equipment before moving to the next phase. Other instruments that work with automated equipment are instruments with hard-to-clean crevices. This equipment uses cavitation and other methods to clean the problematic areas. Automated washing equipment also helps lower the chances of a percutaneous injury.
Instrument washers can help SPD personnel reduce how much they need to handle the instruments. This helps increase the safety of the staff. Before the instruments are moved to the next phase, they should be inspected to ensure no bioburden remains on them. If bioburden is present during sterilization, the instruments will not be able to be sterilized.
Phase 3: Prepping and packing
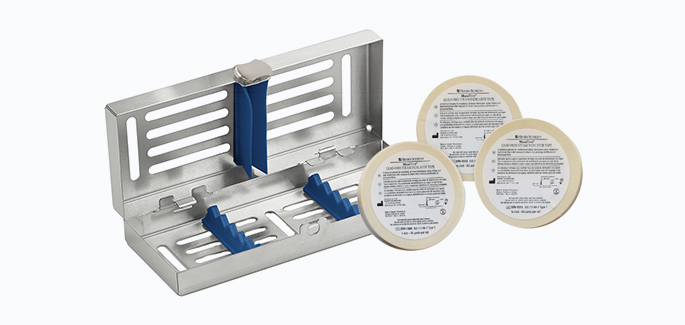
After cleaning, the instruments must be prepped and packed for sterilization. Depending on the procedures and types of instruments, they will be placed in varied sizes and styles of sterilized packaging, instrument trays, and containers. Whichever packaging option the SPD personnel is using, all instructions for use (IFUs) must be followed on how to use the packaging or how to wrap the instrument. SPD professionals must also use the correct chemical indicators that will be placed on the inside and outside of the different packaging options.
If using instrument trays that need central supply room wrap, SPD professionals should use the correct size to cover the entire tray and wrap it securely to prevent gapping or air pockets. Then, SPD technicians must place an accurate chemical indicator on the inside and outside of the tray. These indicators let personnel know if the autoclave sterilized the instruments.
The color on the indicator changes depending on the temperature, time, pressure, and other elements. The instruments are only considered sterile if the chemical indicators change. After the packages are wrapped, labeling is next. Labels can include the date, who processed the instruments, which autoclave was used to sterilize, the cycle or load, and the expiration date, if applicable. After the instruments are prepped and packed, they are ready to move to the next phase.
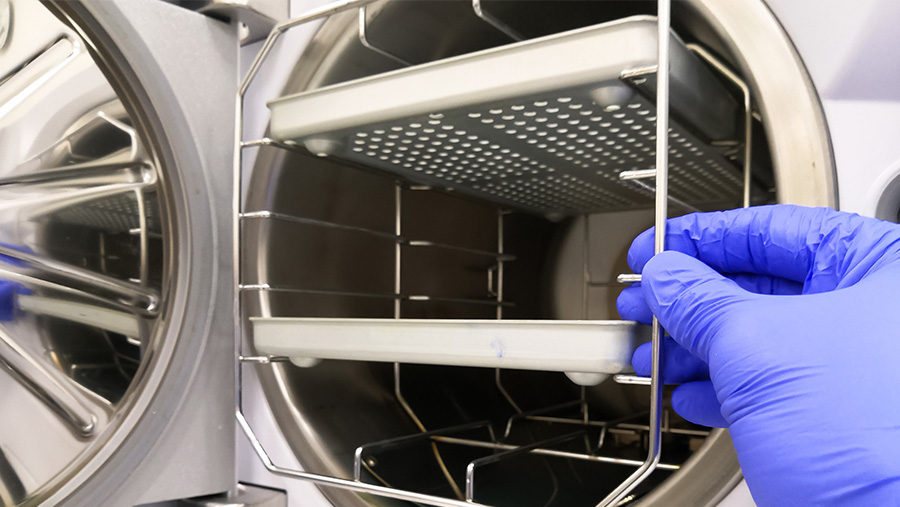
Phase 4: Sterilization
Autoclaves and high-level disinfectants are the two types of sterilization processes. There are also different forms of autoclaves. These include:
• Steam sterilization
• Ethylene oxide
• Dry heat
• Low temperature; and others.
If instruments can withstand heat and/or steam, these instruments can be sterilized through steam or dry heat sterilization. If the instruments/devices cannot withstand heat and steam, they will be sterilized with low-temperature sterilization, ethylene oxide sterilization, and high-level disinfection. This sterilization usually uses a chemical (hydrogen peroxide plasma gas, ethylene oxide, peracetic acid, etc) to sterilize fragile instruments safely. SPD personnel must consistently undergo training and wear the proper PPE around these chemicals, which can be hazardous to the body and, if mishandled, could cause severe harm to the staff.
High-level disinfectants can range from low toxicity to very hazardous. High-level disinfectants do not use autoclaves to sterilize the instruments and devices. Instead, the instruments and devices are placed in only the high-level disinfectant solution to be sterilized. These chemicals could include glutaraldehyde, hydrogen peroxide, ortho-phthaldehyde, and other active ingredients. Because of the toxic nature of some of the active ingredients, SPD personnel must be trained to use and dispose of the chemicals properly. They must also always be in the proper PPE to keep themselves safe. After sterilizing the instruments and devices, they are moved to their final phase.
Phase 5: Sterile storage
Sterile storage helps keep instruments sterile until they are ready for use. The CDC states that sterile instruments and trays must be 8 to 10 inches off the floor, five inches below the ceiling, 18 inches below the sprinkler head, and two inches away from the wall. This will allow the proper airflow throughout the sterile storage area to help maintain sterility.
Monitoring
Even when all phases are complete, there are still other tasks that the SPD must perform throughout the day. One critical task is monitoring. There are several types of monitors/indicators throughout the SPD. These include mechanical, chemical, and biological.
Mechanical Monitoring. Mechanical monitoring requires a physical check of the equipment by the SPD personnel to ensure everything is working.
Chemical Indicators. Chemical indicators are the strips placed inside and outside trays and packaging in order to show that the autoclaves met several parameters. There is also a chemical Bowie Dick test that must be done daily with steam autoclaves. This indicator helps show that the air has been removed during the sterilization process.
Biological Testing. Biological testing shows that the autoclaves can kill spores, ensuring they are sterilized appropriately. Guidelines state that spore testing must be done once a week. However, some infection prevention leaders approve of daily spore tests. If a facility does not want to do a spore test daily, they can use class 5 integrator strips. These simulate what a spore test would show, ensuring the sterilizer is killing spores. However, these do not replace biological spore testing, which must be completed every week. Regardless of the indicators or monitoring, SPD personnel must record every result, including the package indicators from the sterilizer—documenting what is monitored helps keep patients safe. SPD personnel will consistently have records to show if the instruments can or cannot be used, depending on the results of the tests and indicators.
A day in the life of personnel in SPD can be challenging. It requires rigorous training, high-standard policies and procedures, consistency in maintaining the proper steps, and ensuring that all instruments are safe and ready for use in any given surgical procedure. High turnover and staffing shortages can—and do—impact the consistency and maintenance needed to uphold proper sterility in an ASC. However, even with those difficulties, the SPD staff should always follow the guidelines, not only to keep patients safe, but to ensure the safety of the staff, too.
Original Article: https://www.ormanager.com/a-day-in-the-life-in-spd/
Erica Smith, MBA, is a Surgical Solutions Manager at Henry Schein, Inc. In this role, she helps guide ASC healthcare professionals in conducting proper infection prevention protocols. She is currently completing her doctorate in Public Health to advance her infection prevention skills and knowledge.
References
Link T. Guidelines in practice: Sterilization packaging systems. AORN Journal, 2020;112(3):248–260.
Sterilizing practices. Centers for Disease Control and Prevention. Accessed March 2023.
Consult An Expert
Need more specific guidance or tailored product recommendations? Our team of infection control consultants is here to help. Contact us using the form below.